Diabetes is one of the most common chronic conditions worldwide, and while it affects multiple organs, its impact on the feet is often underestimated. Among its serious complications, diabetic foot ulcers stand out as one of the most challenging and potentially devastating problems. Left untreated, these wounds can progress to infections, gangrene, and even amputation.
For patients in Kerala, Diabetic Foot Ulcer Reconstruction Thrissur services at the Sushrutha Institute of Plastic Reconstructive and Aesthetic Surgery (SIPRAS) offer advanced, evidence-based treatments to restore health, function, and quality of life. Located within Elite Mission Hospital, Koorkenchery, Thrissur, SIPRAS combines surgical excellence with compassionate patient care.
Understanding Diabetic Foot Ulcers
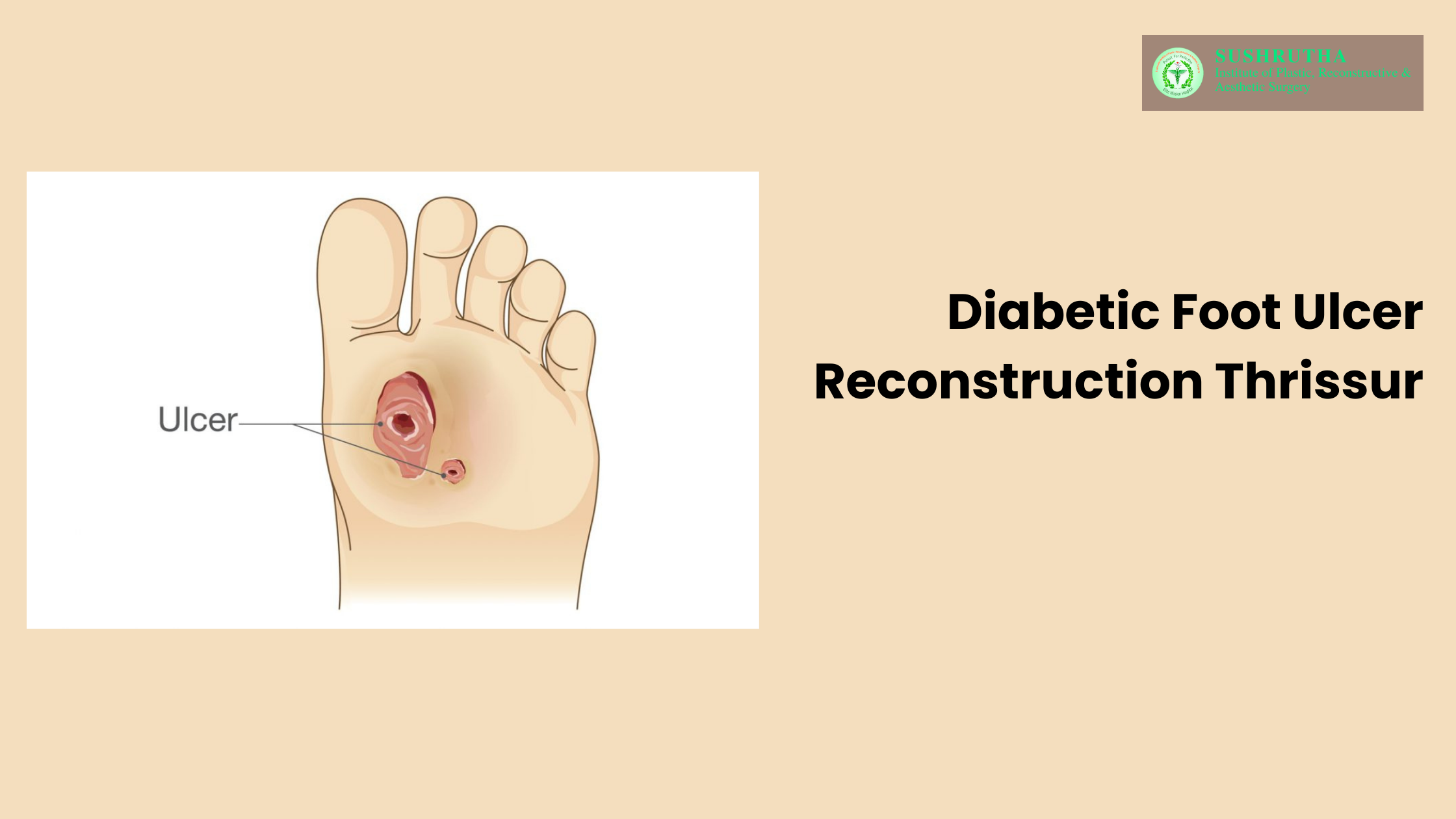
A diabetic foot ulcer is an open sore or wound that develops on the foot — most commonly on the sole — as a result of a combination of poor blood circulation, nerve damage (peripheral neuropathy), and delayed wound healing. In people with diabetes, even a small blister, scratch, or cut can progress into a severe ulcer within days if not treated promptly.
Key Facts:
Around 15% of people with diabetes will develop a foot ulcer during their lifetime.
Diabetic foot ulcers are the leading cause of non-traumatic lower-limb amputations worldwide.
Early diagnosis and intervention significantly improve healing rates, reduce infection risk, and prevent amputation.
At SIPRAS – Sushrutha Institute for Plastic, Reconstructive & Aesthetic Surgery in Thrissur, our Diabetic Foot Ulcer Reconstruction Thrissur services are designed to manage the problem holistically — from accurate diagnosis and advanced wound care to microsurgical reconstruction and rehabilitation.
Why Specialized Care Matters for Diabetic Foot Ulcer Treatment in Thrissur
Treating a diabetic foot ulcer goes far beyond simply dressing the wound. Multiple factors — blood sugar control, infection prevention, vascular health optimization, and biomechanical balance — must be addressed for lasting results.
In advanced cases where ulcers are deep, involve tissue loss, or expose bone, diabetic foot reconstruction becomes necessary. SIPRAS’s Diabetic Foot Ulcer Reconstruction Thrissur unit offers:
Microsurgical expertise for complex wound coverage.
Advanced flap surgeries to restore skin and soft tissue.
Limb salvage procedures to avoid amputation.
Benefits of specialized diabetic foot reconstruction include:
Preservation of limb function and mobility.
Shorter hospital stay and quicker return to daily activities.
Faster healing with lower recurrence rates.
Improved cosmetic appearance and patient confidence.
Causes and Risk Factors for Diabetic Foot Ulcers
Diabetic foot ulcers develop due to a combination of vascular, neurological, and mechanical factors. Understanding these underlying causes is essential for prevention, timely intervention, and successful treatment.
1. Peripheral Neuropathy
Over time, high blood sugar levels can damage peripheral nerves, leading to sensory neuropathy. This results in a reduced or complete loss of pain, temperature, and pressure sensation in the feet. Because of this, small injuries, blisters, or pressure sores may go unnoticed until they progress to more serious wounds. Motor neuropathy may also cause muscle imbalance, altering foot shape and gait, which further increases ulcer risk.
2. Peripheral Arterial Disease (PAD)
Diabetes accelerates atherosclerosis, causing narrowing or blockage of arteries that supply the lower limbs. Poor circulation means reduced oxygen and nutrient delivery to tissues, slowing wound healing and increasing the risk of infection. Even minor injuries can become chronic when blood flow is compromised.
3. Foot Deformities
Structural changes in the foot—such as bunions, hammertoes, and Charcot neuroarthropathy—create areas of abnormal pressure. These high-pressure points can cause skin breakdown, especially in patients who also have neuropathy and cannot feel the developing injury.
4. Uncontrolled Blood Sugar
Chronic hyperglycemia impairs the immune system, delays tissue repair, and promotes bacterial growth. Poor glycemic control is one of the strongest predictors for both ulcer development and poor healing outcomes.
5. Previous Ulcers or Amputation
A history of foot ulcers, infections, or amputation significantly raises the risk of recurrence. Scar tissue is less resilient and more prone to breakdown, while underlying risk factors—such as neuropathy and PAD—often remain present.
At SIPRAS’s Diabetic Foot Ulcer Reconstruction Centre in Thrissur, our multidisciplinary team begins by thoroughly assessing each patient to pinpoint and address these root causes. This comprehensive approach—combining vascular evaluation, neuropathy screening, infection control, and biomechanical correction—forms the foundation before any reconstructive or surgical intervention.
Complications of Untreated Diabetic Foot Ulcers
1. Severe Soft Tissue and Bone Infections
Ulcers provide an entry point for bacteria, which can cause cellulitis, abscesses, and necrotizing fasciitis. In advanced cases, infection can spread to the bone (osteomyelitis), making treatment more difficult and often requiring prolonged antibiotics or surgery.
2. Sepsis
When infection spreads from the foot into the bloodstream, it can trigger a systemic inflammatory response. Sepsis is a medical emergency that can lead to multi-organ failure and death without immediate intervention.
3. Permanent Disability and Mobility Loss
Ongoing pain, chronic infection, or joint destruction (such as in Charcot neuroarthropathy) can severely impair mobility. Reduced activity often leads to muscle wasting, poor cardiovascular health, and increased dependence on others.
4. Lower Limb Amputation
In cases where infection is uncontrolled, blood flow is critically reduced, or tissue death (gangrene) sets in, partial or complete amputation of the foot or leg may be the only life-saving option. Diabetes remains one of the leading causes of non-traumatic amputations worldwide.
5. Reduced Quality of Life and Independence
Chronic wounds and their complications often cause psychological distress, depression, and social isolation. Daily life can become limited by the need for wound care, restricted mobility, and fear of recurrence.
Diabetic foot ulcer reconstruction is a surgical procedure used to repair and restore damaged tissue, skin, or bone in the foot caused by diabetes-related ulcers. At Diabetic Foot Ulcer Reconstruction Thrissur facilities in SIPRAS, this includes advanced microsurgery and skin grafting techniques.
If your ulcer is deep, not healing with conventional wound care, or has caused tissue loss, your doctor may recommend Diabetic Foot Ulcer Reconstruction Thrissur to prevent amputation and restore function.
Healing time varies from patient to patient, but on average, recovery after Diabetic Foot Ulcer Reconstruction Thrissur can take 6–12 weeks, depending on the size of the wound and your overall health.
Yes, most patients regain mobility, especially with proper physiotherapy. The goal of Diabetic Foot Ulcer Reconstruction Thrissur is not only to heal the ulcer but also to help you return to your normal activities.
Procedures may include skin grafts, local flaps, free flaps, or tendon and bone reconstruction. At Diabetic Foot Ulcer Reconstruction Thrissur centers like SIPRAS, the method is chosen based on ulcer size, depth, and location.